|
Related Topics: |
|
|
|
Current News |
|
Chemistry A to Z |
|
About Internetchemistry |
Purdue researchers develop technology to detect cancer by scanning surface veins |
|
Researchers from Purdue's Cancer Center, Department of Chemistry and Weldon School of Biomedical Engineering collaborated with cancer and biotechnology experts from the Mayo Clinic to develop technology to detect tumor cells within the human body. By shining a laser on surface veins, such as those on the wrist and inside the cheek, researchers are able to reveal and count circulating tumor cells. In addition to being less invasive, the new detection method is able to evaluate a much larger volume of blood than what can be drawn from a patient for analysis, said Philip Low, Purdue's Ralph C. Corley Distinguished Professor of Chemistry. "In the initial stages of cancer, there are very few circulating tumor cells - cells that indicate the spread of cancer and initiate secondary tumor formation," Low said. "By increasing the volume of blood analyzed, we improve the sensitivity of the test and allow for earlier diagnosis. If there are two cancer cells in every 50 milliliters of blood, odds are the cells would not be found in a 10-milliliter blood sample. However, the cells would be found in the 100 milliliters of blood that flow through large veins each minute." |
|
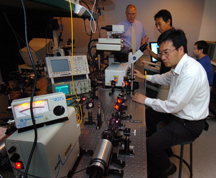
Optical imaging provides high resolution and chemical specificity for cancer detection, but it usually suffers from limited penetration depth, making it hard to reach tumors inside the body, said Ji-Xin Cheng, an assistant professor of chemistry and biomedical engineering. "In vivo detection of circulating tumor cells in surface veins provides an excellent way to overcome this problem," Cheng said. "Circulating tumor cells provide a benchmark for disease progression and precise monitoring of their levels could lead to personalized treatment," Low said. "This technique allows us to quantify the amount of circulating tumor cells present, as opposed to tests that provide a 'positive' or 'negative' result. "Through such precise monitoring, a physician could evaluate the response to chemotherapy and regularly adjust the dosage so that only the exact amount needed would be administered. This could reduce the time a patient is treated and the serious side effects that occur." The technique could provide doctors and patients results in a matter of minutes and save the medical industry millions of dollars in testing equipment, said Wei He, a graduate student in the Department of Chemistry and the Department of Biomedical Engineering. He worked on the project with Low and Cheng. By directly labeling tumor cells while they are in the bloodstream, some of the costs and problems associated with testing drawn blood samples can be avoided, He said. One sample can require five to 10 test tubes during the course of sampling, processing and analysis such as handling, labeling and washing," He said. "In addition, large hospitals can have more than 300 cancer patients in one day. Such a large influx can cause delays in sample processing and delays can affect the results of analysis." A paper detailing the technology and detection technique was published in the July 10 Proceedings of the National Academy of Sciences. In addition to Low, He and Cheng, postdoctoral researcher Haifeng Wang and Lynn C. Hartmann, a professor of oncology and associate director for education of the Mayo Clinic Cancer Center, co-authored the paper. The technique uses a fluorescent tumor-specific probe that labels tumor cells in circulation. When hit by a laser, which scans across the diameter of the blood vessel 1,000 times per second, the tumor cells glow and become visible. The in vivo flow detection was performed on a two-photon fluorescence microscope in Cheng's lab. The researchers compared several methods and found two-photon fluorescence provides the best signal to background ratio. The technology is able to scan every cell that is pumped through the vessel, He said. Low's team has developed two labeling agents that attach to different forms of cancer. One label targets ovarian, non-small lung, kidney and endometrial cancer, and the other targets prostate cancer. These labels would be administered through an injection. The first label has already been tested in humans and has no adverse side effects and could potentially be administered weekly, He said. Computed tomography, or CT, scans and magnetic resonance imaging, or MRI, are the current methods used to track the spread of cancer. These methods have a limited resolution, and a 1 millimeter tumor could go undetected by CT or MRI. The Purdue-developed technology can achieve single-cell resolution and can detect rare cell populations. "Our method can detect cancer cells early in disease development and the test can be conducted frequently," Low said. "Discovering the cancer early and knowing whether it has metastasized, or spread, greatly improves a patient's chance for successful treatment." The laser penetrates to a depth of 100 microns and is able to examine shallow blood vessels near the surface of the skin. Advanced optical technology could be incorporated into the technology platform and enable the method to reach deeper vessels that handle larger volumes of blood, Cheng said. The Purdue team continues to work with the Mayo Clinic and is planning to initiate a clinical trial to further evaluate the technique. The team also plans to develop labels for additional types of cancer and to downsize the equipment to make the technology portable. This research was funded by an Indiana Elks Charities Grant, the Purdue Cancer Center and an Ovar'Coming Cancer Together research grant. |
|
|
|